Ayushman Bharat Yojna
- Home
- Ayushman Bharat Yojna
Ayushman Bharat Yojana Cashless facility at Hopewell Hospital
The Ayushman Bharat Yojana is the biggest health insurance plan in the world. It offers health insurance of Rs 5 lakh to every Indian family that qualifies.
At Hopewell Hospital, we recognize the significance of the Ayushman Bharat Yojana as the world’s largest health insurance plan, providing invaluable support to millions of Indian families. This transformative initiative offers a comprehensive health insurance coverage of Rs 5 lakh to qualifying households, ensuring access to essential healthcare services.
With a reach extending to nearly 50 crore individuals, Ayushman Bharat plays a crucial role in addressing the healthcare needs of approximately 40% of economically disadvantaged families in India. Eligibility for participation in this program is determined based on occupation and socioeconomic status, leveraging data from the Socio-Economic Caste Census of 2011 to identify deserving beneficiaries.
Formerly known as the National Health Protection Scheme, Ayushman Bharat succeeded the Rashtriya Swasthya Bima Yojana established in 2008. Notably, Ayushman Bharat also extends coverage to families previously enrolled in RSBY but excluded from the SECC 2011 list. Financed by the Indian government, this initiative aims to mitigate the financial burden of exorbitant medical expenses, safeguarding families from the threat of impoverishment due to healthcare costs.
At Hopewell Hospital, we are committed to supporting the goals of Ayushman Bharat by providing quality healthcare services to beneficiaries, ensuring that they receive the medical attention they require without facing financial hardships. We are proud to be part of this monumental endeavor to enhance healthcare accessibility and affordability for all.
Key Features of Ayushman Bharat PM-JAY
- A well-defined cover of Rs. 5lakh will be provided to every eligible family, every year.
- The beneficiaries will be permitted to avail primary, secondary, and tertiary healthcare services from any of the empanelled public or empanelled private hospitals.
- The benefits will be entirely cashless and portable. This means that neither would the beneficiary have to wait for reimbursements, nor would their location impact their ability to access healthcare.
- The beneficiaries would be identified on the basis of the same deprivation criteria which were used while conducting the socio-economic caste census. This would help determine their entitlement.
- The principle of cooperative federalism would be strictly followed by giving adequate flexibility to the states in terms of expenditure incurred.
- The payments would be made on a package basis. The total costs, specific services and procedures which can be included in the package would be defined by the government in charge.
- An Ayushman Bharat National Health Protection Mission Council would be set up to facilitate coordination between the central and state governments. This apex body would be chaired by the Union minister for health and family welfare. To know more about Ayushman Bharat Yojana (आयुष्मान भारत योजना), please refer to official website.
- An Ayushman Bharat National Health Protection Mission Council would be set up to facilitate coordination between the central and state governments. This apex body would be chaired by the Union minister for health and family welfare. To know more about Ayushman Bharat Yojana (आयुष्मान भारत योजना), please refer to official website.
- Each state would be asked to create a health agency in order to seamlessly implement the scheme.
- An inter-operable and robust IT platform would be designed under the leadership of NITI Aayog, to make sure that all transactions under the plan remain paperless and scalable
Benefits Cover under PM-JAY
While many government-funded medical insurance schemes limit coverage to Rs 3 lakh, the Ayushman Bharat Yojana, or PM-JAY, extends coverage up to Rs 5 lakh. This includes cashless medical treatment for beneficiaries at both public and private hospitals across India. Eligible families can avail this insurance for defined secondary and tertiary care conditions.
The scheme covers all expenses related to:
- Medical examinations, treatments, and consultations
- Pre-hospitalization expenses
- Post-hospitalization follow-up care for up to 15 days
- Diagnostic procedures and lab investigations
- Costs of medicines and medical consumables
- Non-intensive and intensive care services
- Accommodation benefits
- Medical implantation services when necessary
- Food services during hospitalization
- Treatment resulting in complications
- All out-of-pocket expenses incurred during hospitalization
Whether the hospital is public or private, the insurance provided is entirely cashless. Additionally, beneficiaries receive a transport allowance to cover travel costs during the pre and post-hospitalization period. Daycare treatment facilities are also available within the insurance package.
PMJAY Critical Illness Coverage
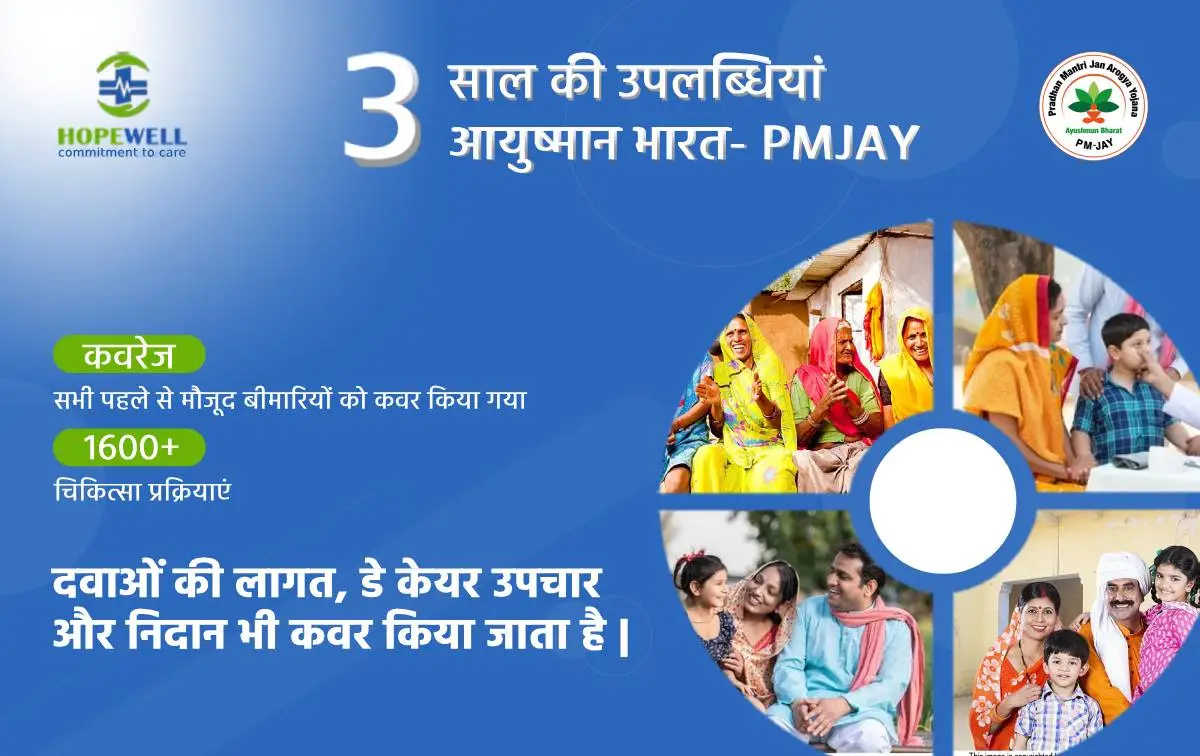
PMJAY provides families access to healthcare services and assistance for daycare procedures, including pre-existing illnesses. The scheme covers nearly 1,350 medical packages at both public and private network hospitals across India.
List of Critical Diseases Covered under Ayushman Bharat Health Scheme
Some of the critical illnesses covered by the policy include:
- Double valve replacement
- Prostate cancer
- Coronary ABG
- Carotid angioplasty with stent
- Anterior spine fixation
- Pulmonary valve replacement
- Skull base surgery
- Laryngopharyngectomy
- Tissue expander for disfigurement in case of burns
Ayushman Bharat Health Scheme has limited exclusions, which include:
- Drug rehabilitation programs
- Outpatient department (OPD) expenses
- Organ transplants
- Cosmetic procedures
- Fertility-related procedures
- Drug rehabilitation programs
- Outpatient department (OPD) expenses
- Organ transplants
- Cosmetic procedures
- Fertility-related procedures
Registration
To register:
- Enlist all individuals and families in the catchment area and update this database regularly.
- Identify and register beneficiaries/families for the Pradhan Mantri Jan Arogya Yojana according to specified criteria.
- Ensure that every family and individual is allocated and informed about their unique Health ID, which will be used for accessing services under various programs.
- Link the unique health ID with the AADHAAR ID, as per government regulations.
- Identify and merge duplicate records by verifying IDs.
- Create a longitudinal health record for each enrolled individual.
Service Delivery
- Record all services provided at the Healthcare Center (HWC) under different programs.
- Enable follow-up of services received by individual patients by recording relevant parameters, diagnostic results, and medications.
- Send SMS/reminders to individuals about follow-up visits.
- Facilitate clinical decision-making for service providers based on standard treatment protocols.
- Track and support referrals to ensure continuity of care.
- Provide key summaries and prescriptions tailored to individual needs.
- Capture, store, and transmit images to support teleconsultation, referral, and follow-up.
Management of Service Delivery
- Capture service delivery coverage and measure health outcomes using population-based analytics.
- Generate work plans for teams, with alert and reminder features for service providers.
- Validate service usage and enable Direct Bank Transfers to beneficiaries as needed.
- Support birth and death registrations and disease surveillance.
- Record other preventive and promotive services delivered, such as vector control.
- Send appropriate Information, Education, and Communication (IEC)/Behavior Change Communication (BCC) messages.
Logistics
- Support inventory management and regular supply of medicines, vaccines, and consumables.
- Maintain a database for equipment at the Healthcare Center to support biomedical equipment maintenance.
Capacity Building
- Provide job aids, such as flow charts or audio/video aids, for continuous learning and support of primary healthcare teams.
- Support access to Massive Open Online Courses (MOOCs) and platforms like ECHO for capacity building and problem-solving for Healthcare Center teams.
Reporting and Monitoring
- Generate population-based analytics reports for routine monitoring and assessing the performance of healthcare providers.
- Create performance matrices for all service providers, calculating incentives from service transaction data in the system.

What is the process to get an Ayushman card?
There is no special registration procedure pertaining to Ayushman Bharat Scheme. All the beneficiaries under PMJAY are either a part of RSBY Scheme or are identified by the SECC 2011. Mentioned below is how you can check your eligibility as a PM-Jay beneficiary. Visit the official website and click on Am I Eligible Provider your mobile number and the CAPTCHA code and click Generate OTP Then select your state and search by mobile number/HHD number/name/ ration card number Based on the results that appear in search you can check if your family is covered under Ayushman Bharat Scheme On the other hand, if you want to check your eligibility under PMJAY you check the Empanelled Health Care Provider or dial the PMJAY helpline number i.e. 14555 or 1800-111-565
Documents Required to Apply For Ayushman Bharat Yojana Scheme
- Age & Identity Proof (Aadhaar Card/PAN Card)
- Contact details (mobile, address, email)
- Caste certificate.
- Income certificate (maximum annual income to be only up to Rs. 5lakh
- Document proof the current status of the family to be covered (Joint or nuclear)
What are the documents that should be considered for addition of a family member in ayushman Bharat Pmjay scheme?
Documents Required to Apply For Ayushman Bharat Yojana Scheme:
- Identity and Age Proof (Aadhaar Card/PAN Card)
- Details of your mobile number, email address and residential address.
- Caste certificate.
- Income certificate.
- Documents stating your current family status.
What are the benefits of PMJAY Scheme?
Ayushman Bharat Yojana benefits include health insurance coverage of up to INR 5lakh per family, annually. Here, all the pre-existing illnesses are covered without any waiting period.